Cardiovascular disease, cholesterol, and your health
Cholesterol has many uses within the body, and we get it either through dietary sources or by our own body’s production. In fact, human body manufactures 60 – 75% of its total cholesterol for its own use. The body uses cholesterol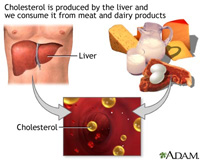 as a sort of “glue” to keep cell membranes from falling apart, and is one of the building blocks for many of the body’s hormones such as estrogen, testosterone and cortisone. In the intestines, the cholesterol is a large constituent in bile which emulsifies fats and allows them to be absorbed into the body. Recent studies have suggested that cholesterol may have a role in cell signaling and even antioxidant properties.
as a sort of “glue” to keep cell membranes from falling apart, and is one of the building blocks for many of the body’s hormones such as estrogen, testosterone and cortisone. In the intestines, the cholesterol is a large constituent in bile which emulsifies fats and allows them to be absorbed into the body. Recent studies have suggested that cholesterol may have a role in cell signaling and even antioxidant properties.
High blood cholesterol levels seem to lead to the development of artery and heart diseases, but low cholesterol levels can be destructive to the body, with some recent studies suggesting a correlation between cancer risk and low cholesterol. The important aspect here is having a good, healthy balance with respect to cholesterol.
Cholesterol and arteries
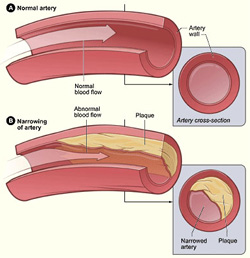 In the lining of the larger arteries, excess cholesterol is deposited in pockets called “plaques” which will often become replaced with calcium over time. This process decreases the lumen size of the vessel and prevents the arteries from expanding and contracting normally, forcing the heart to work harder to pump blood through the body. Consequently, blood does not flow efficiently, limiting the nutrition and oxygen available to tissues and can lead to stroke, heart attack, high blood pressure and circulation problems in the legs and arms. Many studies have found that lowering high cholesterol levels can actually reduce the size and number of plaques and lower the risk of heart attack and stroke. With diligence in changing dietary patterns, this process can be halted and even reversed.
In the lining of the larger arteries, excess cholesterol is deposited in pockets called “plaques” which will often become replaced with calcium over time. This process decreases the lumen size of the vessel and prevents the arteries from expanding and contracting normally, forcing the heart to work harder to pump blood through the body. Consequently, blood does not flow efficiently, limiting the nutrition and oxygen available to tissues and can lead to stroke, heart attack, high blood pressure and circulation problems in the legs and arms. Many studies have found that lowering high cholesterol levels can actually reduce the size and number of plaques and lower the risk of heart attack and stroke. With diligence in changing dietary patterns, this process can be halted and even reversed.
When testing cholesterol levels, the doctor will take a blood sample and order a “lipid profile” which lists the proportions of a number of different fats in the blood. LDL’s and VLDL’s are “bad guys” – proteins which carry cholesterol through the body and deposit excess in the arteries. HDL is the “good guy” – and have been found to carry cholesterol from other sites in the body (including arteries) to the liver where they are made into bile or broken down and used by the body in other areas. The number that the doctor will most often give you is all the types added together – total cholesterol. The doctor also measures the triglycerides in the body, but high levels seem to correlate even more highly with an increased risk of diabetes, than heart disease. These levels are best lowered by removing sugar and other refined carbohydrates from the diet.
There is some disagreement among various sources about the levels of the LDL’s VDL’s and HDL’s that are considered optimal for health. Based on present research, we prefer total cholesterol to be between 150 & 190mg/dl HDL’s should be 1/3 to 1/2 the total cholesterol. Because 60-75% of the body’s cholesterol is produced by the body, even with a cholesterol-free diet one could still be in the cardiovascular danger zone. In most cases however, a few changes in diet will significantly lower the blood cholesterol levels. There are other factors that can affect cardiovascular risk, such as homocysteine, and C-reactive protein, and studies have been suggesting that these and other cardiovascular risk factors are even more accurate in determining the risk for a cardiovascular event.
What can I do about my cholesterol level?
The first and most obvious change one may make is to decrease the intake of cholesterol into the body. Animal fats and dairy products such as butter, cheese and egg yolks all contain cholesterol in large quantities. Plants do NOT contain cholesterol. Even though you are decreasing the intake of cholesterol, you must be sure that you are eating enough protein – an average person needs two ounces daily. Good sources of protein with low cholesterol content are fish, lean beef, skinless chicken, beans, grains and nuts.
What about fats?
The body builds cholesterol most quickly from saturated fats and decreasing these will reduce levels as well. Saturated fats are the solid-at-room temperature ones such as animal fats, plant oils that have been hydrogenated to make them solid (margarine & shortening) and coconut and palm oils. Saturated fats raise cholesterol twice as much as polyunsaturated fats (oil-at-room-temperature fats). Unsaturated fats should be retained in the diet. Olive oil is known to raise beneficial HDL levels while saturated fats lower it. Fatty acid oil components are needed for hormone synthesis, skin function, cell wall synthesis, and other cellular processes. The best kinds of oils are cold-pressed soy, sunflower, safflower, nut and flax seed oils.
solid (margarine & shortening) and coconut and palm oils. Saturated fats raise cholesterol twice as much as polyunsaturated fats (oil-at-room-temperature fats). Unsaturated fats should be retained in the diet. Olive oil is known to raise beneficial HDL levels while saturated fats lower it. Fatty acid oil components are needed for hormone synthesis, skin function, cell wall synthesis, and other cellular processes. The best kinds of oils are cold-pressed soy, sunflower, safflower, nut and flax seed oils.
What else can I do?
Besides reducing intake, another way to lower cholesterol levels is to increase its elimination from the body. This means more fiber in your diet. Cholesterol containing bile is secreted by the liver and carries fat to the side of the intestines where the fat is absorbed. The bile is then reabsorbed just before the small intestines empty into the large intestines. If the re-absorption of bile is reduced, it gets excreted in the feces along with the cholesterol it contains. The liver will then use stored cholesterol to make new bile. Oat bran and apples are especially good absorbing agents, but evidence suggests that increasing fiber of any kind in the diet will decrease cholesterol levels. We define fiber as the undigestible cell walls of the plants that travel through the gut unchanged, so that any whole, unrefined plant will work – vegetables, grains and beans. The process of refining grains removes most of the fiber. Use whole grains and be liberal with consumption of beans. Half-a-cup serving of cooked pinto or navy beans daily can lower LDL cholesterol levels by 20%. One tablespoon of ground flax seeds mixed in yogurt or dilute fruit juice in the morning can also be beneficial.
Cardiovascular Risk Factors and Micronutrients
During the 1960s and ’70s, research scientists examined the relationship between micronutrient deficiencies and heart disease, but it wasn’t until recently (the past 10 years), when research steadily accumulated with results so compelling,  many clinicians now include nutritional intervention in their treatment and prevention of this disease. This exciting research confirms what earlier scientists suspected: vitamin deficiencies contribute to the processes leading to the development of cardiovascular disease. These include B6, B12, and folate which are required for proper homocysteine metabolism. Intracellular deficiencies of these specific B-vitamins are responsible for 70% of the cases for hyperhomocysteinemia. Other micronutrients include calcium and magnesium for their role in maintaining the normal function of the heart muscle; antioxidants for their role in scavenging free radicals which have been shown to cause cellular damage contributing to heart disease, and a number of other micronutrients.
many clinicians now include nutritional intervention in their treatment and prevention of this disease. This exciting research confirms what earlier scientists suspected: vitamin deficiencies contribute to the processes leading to the development of cardiovascular disease. These include B6, B12, and folate which are required for proper homocysteine metabolism. Intracellular deficiencies of these specific B-vitamins are responsible for 70% of the cases for hyperhomocysteinemia. Other micronutrients include calcium and magnesium for their role in maintaining the normal function of the heart muscle; antioxidants for their role in scavenging free radicals which have been shown to cause cellular damage contributing to heart disease, and a number of other micronutrients.
Homocysteine, Lipids and Proteins
In addition to well-known risk factors, other proatherogenic factors have been identified which contribute to the development of atherosclerosis:
- Elevated homocysteine status
- Elevated LDL cholesterol (the “bad” cholesterol)
- Elevated lipoprotein(a) status
- Elevated c-reactive protein status
- Elevated apolipoprotein B status
- Low apolipoprotein A-1
- Low apolipoprotein B
- Low HDL cholesterol (the “good” cholesterol)
For more detail about what these factors are, click here.
Medical findings support the health benefit of laboratory testing to improve the assessment of risk, particularly in persons with a personal or family history of cardiovascular disease. Coronary heart disease is the number 1 cause of fatality in the U.S.; stroke is number 3, and the leading cause of serious, long-term disability. But early detection and treatment can make a big difference in reducing cardiovascular risk and thus, improving one’s health.
Studies have associated moderate elevations in homocysteine with coronary heart disease, MI, cerebrovascular disease, carotid intima-media thickness, lower extremity arterial disease, and isolated systolic hypertension. Since homocysteine metabolism depends on B vitamins as cofactors, the relationship between B vitamin status, homocysteine levels, and atheroclerosis has been the focus of many investigations. Early detection of deficiencies is a critical step in disease prevention. At Desert Naturopathic Health, we have a cardiovascular profile which includes homocysteine, and can detect functional deficiencies of vitamins B6, B12, folic acid, calcium, and magnesium, as well as total antioxidant function.
At Desert Naturopathic Health, we can perform these important tests and others to determine a very accurate cardiovascular assessment, and in turn, a very comprehensive treatment plan. Please call us if you have questions at 602-888-1201.
